» Gastroenterology

Secret signs of reflux
People with CdLS may not show the ‘normal’ symptoms of gastro oesophageal reflux disease (GORD) but, according to a new study, the number of patients with the disorder is much higher than previously expected.
For many years the Foundation has urged parents to ensure a test for ‘reflux’ is done as a standard. Many have reported back that doctors have said there is no point as their child is not showing signs of reflux.
GORD, or reflux, is defined as an abnormal return of acid gastric material into the oesophagus because of the bad function of the cardias (the valve that is supposed to stop anything coming from the stomach into the oesophagus). Everybody in the general population has reflux at some time, with 6 per cent of all adults and 11 per cent of babies under one year showing excessive signs or a pathological disease (GORD).
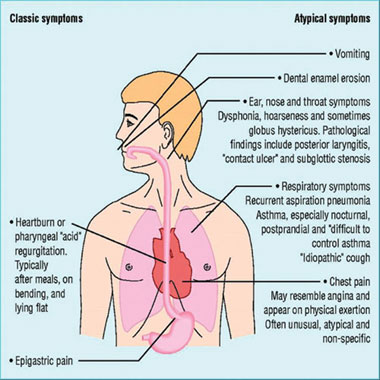
Symptoms
The typical symptoms of excessive GOR usually recognised by GPs include vomiting, regurgitation, refusal of food and frequent airways infections. However, the new research shows that many CdLS people show atypical symptoms such as bruxism (teeth grinding), nocturnal agitation, hyperactivity, and self injurious behaviour (SIB).
Scientific Advisory Council (SAC) member, Dr Angelo Selicorni, revealed the results of the research in advance of publication to CdLS families at the Connections meeting at Kilkenny, Ireland last month. Selicorni worked on the research with Dr S. Luzzani, Dr A.Valadè, and Dr F Macchini in Milan, Italy.
Speaking at the meeting, Dr Selicorni said that many of the previous studies of people with CdLS being affected by GORD were on small numbers of patients. Only that conducted by SAC member, Anne Marie Sommer, looked at as many as 17 patients. The Italian research project involved a study of some 43 patients who have a confirmed diagnosis of CdLS. The doctors set out to answer three questions:
- Is GORD really a frequent complication of CdLS in a large number of the people affected?
- Is there any correlation between the CdLS phenotype and GORD?
- How important are behavioural symptoms?
The study involved evaluation of 43 CdLS patients – 18 defined as classical and 25 as mild. The age range was from one month to 30 years and there were 18 males and 25 females.
The doctors carried out a 24-hour pH probe study on 41 of the patients; they did a GI endoscopy on 43 patients and a GI X ray evaluation on 23 patients.
The results showed that two out of every three people tested showed signs of having been affected by GORD.
The chances of suffering from reflux were equal whether the CdLS person was affected mildly or classically. However, the results showed that people defined as classical were nine times more likely to have severe reflux problems and mildly affected CdLS people were three times more likely to show slight reflux problems.
“The incidence of GORD is quite similar in the two different classes, yet the severity of GORD is strictly related to the severity of the CDLS phenotype,” Dr Selicorni said.
The research showed that while only 53 per cent of the people affected showed typical symptoms, such as vomiting, some 83 per cent showed ‘atypical’ symptoms, such as hyperactivity. Half also showed problems at night, with poor sleeping patterns.
The findings were reinforced by Professor Chris Oliver, who said that in his behaviour studies the research team had noted a number of children showing signs of hyperactivity, back arching and self injurious behaviour that subsequently could be seen as indicating reflux. “It is a serious problem that needs to be considered,” Professor Oliver told families at Kilkenny.
Dr Selicorni and the team will be arguing that there is a strong correlation between the behaviour issues and GORD. They believe that this needs to be noted by other paediatricians and by carers.
The Italian doctors went on to see what happened if treatment was carried out on the people affected and their research will prove that medical and/or surgical therapy eases GORD and improves related behavioural symptoms dramatically.
Search
“A careful search for GORD should be performed in every CdLS patient but especially when he or she demonstrates behavioural symptoms,” Dr Selicorni told parents.
With the study group they found that 61 per cent (17 of the 28 CdLS people who showed they were affected by GORD) could undergo medical (i.e. drug) treatment. The remaining 11 patients had too many problems and required surgical intervention.
Dr Selicorni said that these 11 patients underwent surgical correction using the Boix-Ochoa technique (see panel). They were six male and five female patients with an age range from one to nine years. Of the CdLS phenotype: nine were classical (82 per cent) and two mild (18 per cent).
Apart from one patient, all operations were successful. The one patient who had problems was suffering from long-term respiratory complications. These have now been solved.
“The surgical approach is safe and effective in solving these situations,” Dr Selicorni told parents. The Italian doctors have continued to monitor the patients and have noted continual improvements.
The key messages from Dr Selicorni, and reinforced by the CdLS Foundation, are:
- All CdLS children should be checked for oesophageal reflux even if they don't show the normal symptoms.
- Failure to treat reflux could lead to further problems, including ulcers and cancer of the oesophagus. This can be fatal, although it often isn't.
- Even mildly affected children can suffer from GORD but may not show symptoms.
- All GORD can be treated either by drugs or by surgery. The surgery is proved to be safe.
Literature about CdLS has often talked about GERD rather than GORD. This is because of the spelling of oesophagus. American spelling omits the first ‘o’.
UK doctor says don't panic
Leading UK consultant paediatric gastroenterologist, Peter Gillett, says parents shouldn’t be panicked into unnecessary invasive tests to check out GORD.
“Tests are often unnecessary and a careful search for symptoms – typical or not – should be taken before any appropriate tests are done (pH, endoscopy or barium although the latter, as a test for reflux, is not great). Invasive tests are not desirable in any patient if they are not needed.
“My indication for fundoplication is failure of aggressive medical treatment or respiratory complications of reflux like pneumonia, if these don’t settle with medical treatment.”
Speaking at Peebles last year, Dr Gillett warned that fundoplication is not without complications. Problems include loosening of the ‘wrap’ and then patients need to go back onto medication. “There are number of CdLS parents who can attest to this,” Peter says. There are also problems with ‘dumping’ – a bloating or retching against the closed valve at the junction.
Peter says the biggest problem facing parents is getting to see the appropriate person and recommends they get referred to a paediatric gastroenterologist.
Difference in techniques
Dr Selicorni said that people with GORD in Italy underwent surgery with the Boix-Ochoa technique. This is a fundoplication operation (effectively where a wrap is put around the faulty valve to force acid back into the stomach). In the UK and the USA the Boix-Ochoa technique has been replaced by the Nissen Fundoplication since 1993.
In a study into the two techniques at Booth Hall Children’s Hospital Manchester, surgeon, Subramaniam R. Dickson, reported that in a study of 109 fundoplication operations anti-reflux surgery is beneficial in children with significant gastro oesophageal reflux, irrespective of their neurological status, although complications are more common in patients who are neurologically impaired. Nissen fundoplication is more effective and has fewer complications than Boix-Ochoa, the doctors said.